ZOLL Billing is a cloud-based EMS software solution that enables revenue cycle professionals to turbo-charge billing performance, streamline workflows, and deliver more revenue.
Achieve Exceptional EMS Billing Performance, Value, and Interoperability
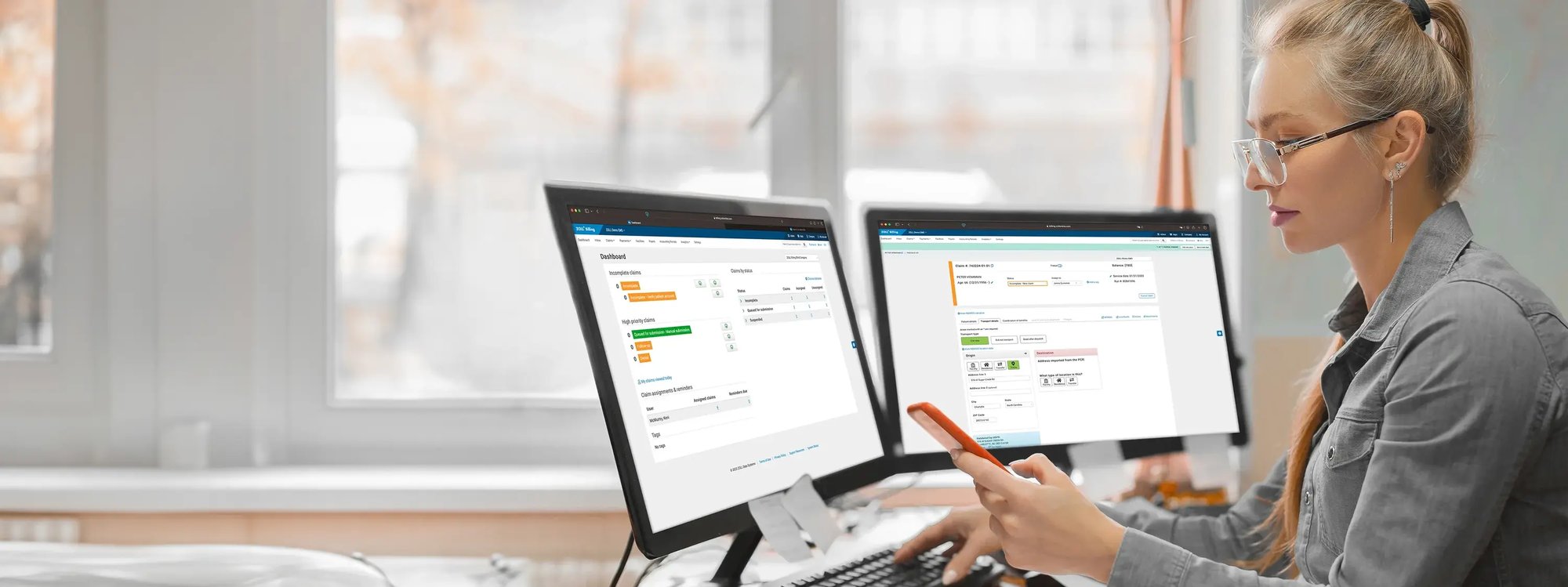
Effective revenue cycle management is essential for a thriving medical services operation. Controlling costs, increasing productivity, and accelerating reimbursements are essential activities that keep EMS agencies rolling. Yet efficiently progressing a claim through its lifecycle has traditionally been labor-intensive and prone to delays caused by documentation and coding inaccuracies, payer-specific documentation requirements, and manually preparing and batching claims for the clearinghouse. By automating workflows and pre-empting billing errors, ZOLL Billing helps you process more claims with fewer resources and address compliance risk at the same time. Built-in, automated accounts receivable (AR) optimization tools verify patient demographics, discover hidden coverage, determine eligibility, and help you partner with self-pay patients to improve collections.
ZOLL Billing integrates pre-billing activities, claims processing, and Medicare coding into one powerful tool that creates logical workflows and makes it easy to process accurate claims faster. Built-in AR optimization tools verify patient demographics and insurance coverage/eligibility to maximize reimbursement and increase self-pay and high-deductible collections. Claims are routed properly, and billing lag is kept to a minimum. And since ZOLL Billing is cloud-based, it securely backs up data continuously and updates itself whenever Medicare codes change. You can rest assured that critical data is safe in case of power outage or loss of network connection and is shielded from cyber-threats.

Featured Case Study
Are you ready to deliver more revenue faster and drive efficiency throughout the claim lifecycle?
