Meet the New ZOLL Dispatch and ZOLL Respond CAD Solution
EMS and Healthcare in 2019: A Glimpse into the Future
I hope everyone had a great holiday season and a positive start in this new year

I hope everyone had a great holiday season and a positive start in this new year.
In last month’s blog, we reviewed several key events and topics that impacted EMS in 2018. This month let’s highlight a few data and technology trends that will continue to evolve within EMS and healthcare in 2019.

The Boundaries of Software and Devices are Merging
Each year, the boundary between software and devices becomes more blurred. The movement toward cloud based (software as a service) solutions, and the development of smart devices that are personal, monitor, diagnosis, collect data and provide real-time analytics will continue to drive EMS and all of healthcare.
Through these devices and software, people-centered care, as described in the EMS Agenda 2050 will begin to emerge.
FirstNet
EMS will widely be able to access FirstNet, the nation’s new public safety communications platform. FirstNet will provide the connectivity and bandwidth to empower data, telemedicine, and secure communication.
Operational and Clinical Outcomes
Data will continue to be critical to EMS operations and clinical care. That being said, there will be increasing challenges in how to manage, analyze, and apply it.
With a new version of NEMSIS (V3.5) arriving in 2019, there will be more emphasis on outcomes. There are also several initiatives underway to automate data transmission and analytics within specialty registries such as CARES and the American Heart Association’s “Get With the Guidelines” quality improvement programs.
Interoperability and Health Information Exchange
Another key to success for EMS in 2019 will be interoperability with other healthcare providers and electronic health records. Standards such as HL7 and IHE, along with regional, state, and national health information exchanges will allow EMS to better exchange important patient demographic and health information.
Although Interoperability is improving for EMS, there is still much work to be done.
Data and Analytics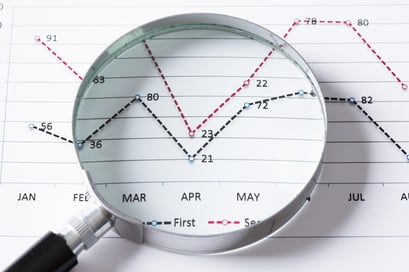
Another area of improvement coming in 2019 to EMS is in the area of analytics. I mentioned that the amount of data and the number of data sources will grow significantly.
To get meaningful and timely information from the data requires the correct analytic software that is user friendly. Dashboards, analytical, and other informational reports should have the ability to be scheduled and alert the user based on the users needs across multiple types of devices.
Communication
Along with FirstNet, EMS communications will continue to evolve in 2019. With the increased bandwidth, telemedicine will gain more traction. More EMS agencies will move from notebook computers to smartphone or tablet-based communication (voice, SMS, video, GIS) tools.
The number of devices and implantation models will vary, but the individual cost will be significantly less.
Clinical Decision Support Will Become More Prevalent
EMS is one area of healthcare that has a great opportunity to implement clinical decision support. Clinical decision support is very much like an automated protocol or treatment guideline. The goal is to help streamline the documentation process and provide feedback or guidance as appropriate.
It can also be effective in standardizing care, improving quality, and reducing errors across a large workforce.
Payment Reform Will Continue to Evolve
 Payment reform for EMS and healthcare will continue to evolve in 2019. Revenue management software must continue to improve to take as much of the guesswork out of managing both personnel and financial resources efficiently and effectively.
Payment reform for EMS and healthcare will continue to evolve in 2019. Revenue management software must continue to improve to take as much of the guesswork out of managing both personnel and financial resources efficiently and effectively.
The number of payer’s that will reimburse EMS for non-transport or non-emergency department transports will continue to increase. Reimbursement for community paramedicine and mobile integrated health services will also improve.
In Conclusion
2019 will be an active and interesting year. Change within technology, EMS operations, clinical care, reimbursement, and policy will continue to progress in parallel, although at difference paces.
I look forward to seeing your comments, additional ideas, and feedback.
Related Posts
Collect More Revenue Faster: The Pivotal Role of Clear, Concise, and Complete Documentation
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS & fire, hospital, or AR professional easier.
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS, fire, hospital, or AR professional easier.




