Integrating EMS into the Healthcare System - Part 1 of a 3 Part Series
Welcome to part one of a three-part series focusing on healthcare reform and the future of Emergency Medical Services (EMS)
Welcome to part one of a three-part series focusing on healthcare reform and the future of Emergency Medical Services (EMS). In the near future, a second post, we will explore how integration of healthcare systems and health information exchange (HIE) will bring new opportunities for EMS operations and clinical care. Finally, in a third post, we will explore a vision of the future, where a patient centric learning healthcare system will forever change EMS and healthcare as we know it.
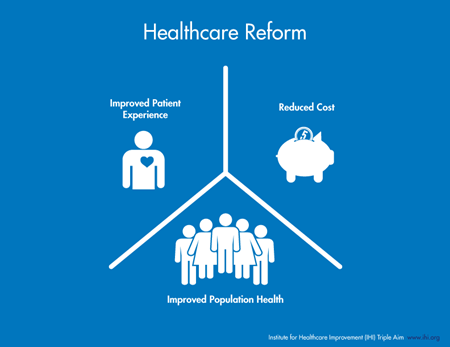
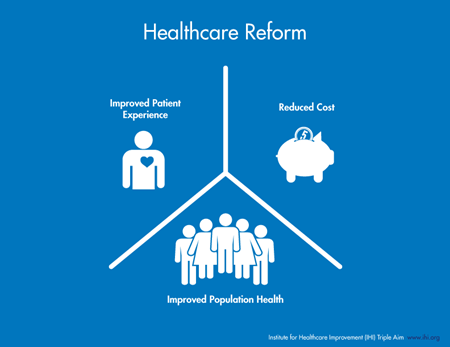
The Triple Aim
Healthcare reform is frequently defined by the triple aim, first coined by the Institute for Healthcare Improvement. The concept is a paradigm shift for the United States compared to mature healthcare systems in other parts of the world. The goal is to focus on prevention and primary care, keeping patients healthy, before they become ill. The three goals of the triple aim are to improve the patient experience (outcome and satisfaction), focus on population health (public health and prevention), all while controlling/decreasing cost. Whether it be heart disease, cancer, diabetes, or any other serious or chronic health condition, the goal is to identify the healthcare risk early and manage it before it becomes life altering or threatening. Once a patient becomes symptomatic, the battle is often lost. Each year, more than 80% of US healthcare dollars are expended on 20% of its patients; those who become acutely symptomatic and ill from a preventable or controllable condition, often going for years (if not decades) without a preventative health plan, or regular/organized primary care.
In 2010, the Affordable Care Act was passed with a vision of universal healthcare coverage and access. However, healthcare delivery is complex: Having a goal of universal healthcare coverage does not by itself mean improved healthcare delivery and patient outcomes.
Where Does EMS Fit into the Triple Aim?
So where does EMS fit into this vision of healthcare reform, how does it change the approach and services EMS delivers, and most importantly, how can EMS maximize its contribution to the triple aim?
EMS is the only acute healthcare provider where the care is physically delivered to the patient, as oppose to the patient physically traveling to the healthcare provider. EMS is one of the few healthcare entities where it is impossible to separate operations from clinical care. EMS also benefits from a respected history within a community, providing opportunities to engage patients and promote population health and prevention. Over the past several years, EMS Mobile Integrative Health and Community Paramedicine (MIH/CP) has evolved, meeting these new and evolving needs. Currently, healthcare reimbursement models force MIH/CP implementations to be creative from a funding perspective. Despite this funding challenge, programs such as REMSA (Reno, NV) and MedStar (Ft. Worth, TX) have shown both an outcome and fiscal benefit to patients and communities.
Integration & the Role of Interoperability
Beyond traditional EMS system implementations and MIH/CP programs, healthcare reform will bring significant and meaningful improvements to EMS. Each of the new healthcare delivery and payment models will require a more integrated approach from a data, care delivery, and coordination perspective. This is where EMS will finally be adopted, accepted, crowned, and rewarded as a formal member of the healthcare community. This integration (often referred to as interoperability) requires each patient event to be viewed as a continuous event, inclusive of all healthcare providers. For example, a STEMI patient is not just an EMS run; it is an integrated “episode of care” beginning with the 911 call, through the EMS response and care, transport to the appropriate healthcare facility, PCI intervention, rehabilitation, and the 90-days post event where the patient returns (as near as possible) to their functional position within the community. Just as the chain of survival for cardiac arrest is linked to positive outcomes, the chain of integration/interoperability for each patient’s “episode of care” is linked to positive outcomes in healthcare reform.
True integration/interoperability requires coordination and communication between EMS and its healthcare systems. For EMS to successfully make its full contribution to the triple aim, we must focus on two key healthcare delivery components: patient navigation and the access of each patient’s healthcare information. In any one community, 30% to 50% of the population receive their healthcare from more than one healthcare system. Key requirements for triple aim success include making the best decision on when and where to transport a patient (based on the patient’s condition and need), keeping a patient within their primary care/healthcare providers network (patient navigation), reducing repetitive healthcare diagnostics (repeat labs, CT scans, etc.), and preventing medical errors (medication errors, adverse reactions, protocol decision errors, etc.). The ability to access each patient’s health record during an EMS patient care event is critical to reducing errors and controlling costs.
In part two of this three-part series, we will explore how HIE (the ability for EMS to view a patient’s health record at the time of care) is critical to the success of healthcare reform. We will also review the four key EMS use cases where HIE directly impacts operational and patient outcomes.
Related Posts
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS & fire, hospital, or AR professional easier.
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS, fire, hospital, or AR professional easier.




